At the frontier of scientific exploration, few fields captivate the imagination like neurotechnology. With its promise to decode the mysteries of the nervous system, neurotech holds the potential to revolutionize how we treat disease, enhance human capabilities, and better understand ourselves. Achieving these breakthroughs is not about taking small steps, but daring to leap and embarking on moonshots that challenge deeply held assumptions to push the boundaries of possibility. However, we must be mindful of the human tendency for old ideas to lead to confirmation bias. This can limit our ability to see beyond current assumptions in creating better applications.
It’s a dogma-eat-dogma world
The history of neuroscience is replete with examples of long-held beliefs that were eventually overturned. Examples include the “single neurotransmitter dogma” that each neuron produces only one type of neurotransmitter, or the “static adult brain myth” that adult brains do not grow new neurons. These serve as reminders of the importance to challenge established beliefs and remain open to new possibilities. To achieve moonshot breakthroughs in neurotechnology, we must question the very foundations of knowledge. Current paradigms, no matter how established, should be scrutinized with a critical eye.
Strategies to facilitate disruptive innovation
1. Create a space open to new ideas
To foster truly innovative moonshots in neurotechnology, we must create intellectual and experimental spaces for new ideas to flourish. This requires a willingness to challenge current limitations and question beliefs or assumptions that may be preventing exploration of new avenues. For example, are we overly focused on neuron-centric models at the expense of understanding the role of glial cells in cognition? And, if so, are we using the understanding of different types of neurons to develop more precise and effective treatment options? Keeping these nuances of cells in mind may enable more seamless integration with the nervous system while keeping it in balance.
We must also embrace complexity and recognize that biological systems, especially the human brain, operate in intricate and nonlinear ways. This calls for interdisciplinary approaches that can capture this complexity, such as integrating insights from chaos theory, network science, or quantum biology.
Researchers must also be open to exploring alternative paradigms and actively pursue other explanations or mechanisms for observed phenomena. For example, whether consciousness can arise from quantum effects in microtubules within neurons, as proposed by Hameroff and Penrose’s Orch-OR theory.
2. Hold onto ideas, but not too hard
It is crucial to cultivate a mindset of intellectual humility and flexibility, in order to avoid the pitfalls of confirmation bias and dogma. Constantly questioning our own assumptions and probing potential flaws in our theories, can identify blind spots in our thinking and open new avenues for exploration. At the same time, encouraging constructive skepticism can foster a research culture that values and rewards thoughtful criticism and alternative viewpoints, rather than confirmatory results.
We must also be open to considering multiple hypotheses and actively explore alternative explanations or mechanisms, no matter how unlikely they may seem at first. This approach, the method of multiple working hypotheses, can lead to unexpected insights and breakthroughs. One example is in neuroplasticity. Despite the Hebbian rule of “cells that fire together wire together,” staying open to the possibility of other forms of plasticity has allowed people to find that there are other plasticity rules, such as anti-Hebbian and homeostatic plasticity. With multiple ways for the nervous system to undergo changes, these mechanisms might be leveraged for therapeutic development.
3. Embrace an integrative approach inside and out
Embracing an integrative approach to neurotech can open a new frontier of innovation and the introduction of groundbreaking solutions to address neurological disorders and advance human health. By recognizing the intricate connections between the brain and other bodily systems, such as the gut-brain axis and neuroimmune interactions, we can develop more holistic and effective interventions.
This approach, leveraging insights from bioelectricity, the autonomic nervous system and neurocardiology, can create comprehensive solutions that address the complex interplay between neural and physiological processes. This presents an unprecedented opportunity for neurotech innovators and entrepreneurs to tap into previously unexplored markets, positioning their organizations at the forefront of a transformative wave in medical technology and human augmentation.
Neurotechnology is inherently interdisciplinary, encompassing a wide range of disciplines, including biomedical engineering, computation, and interaction design. Many discoveries and innovations in neuroscience came about through bringing perspectives from other fields. For example, Sonera and NeuroBionics are both leveraging advances in materials science, specifically magnetic resonance imaging (MRI) to improve neural interfaces. While MRI developments did not begin in neuroscience, its origins in physics, engineering, and radiology have helped to chart the nervous system.
Daring to question deeply held beliefs and dreaming big can pave the way for extraordinary advancements – moonshots for those willing to break from conventional thinking and chart new paths into the unexplored territories of the human mind and brain.
Charting the course for moonshots
The next great leap in neurotechnology may not come from incremental improvements to existing approaches, but a paradigm shift that completely reframes how we think about the brain and mind. These strategies offer a framework to push the boundaries of possibility. Challenging ourselves to question assumptions, explore alternative explanations, and collaborate across disciplines in unprecedented ways can open up the possibility of new breakthroughs. These moonshots may revolutionize our understanding of the brain, leading to transformative treatments for a range of neurological and psychiatric conditions.
This article was originally published on February 2nd, 2025, via DotMed
HERZLIYA, Israel, Jan. 28, 2025 — Corundum Neuroscience (CNS), a leading neuroscience venture builder and fund, today announced the appointment of Itsik Francis, PhD, as Head of Business Development. The appointment comes as the company continues to expand its portfolio of neurotech ventures and strategic partnerships.
With more than 15 years of experience spanning investment and business development in the medtech and biotech sectors, Francis will focus on driving deal flow and investment strategies to propel Corundum Neuroscience’s portfolio growth. He will also provide targeted support to portfolio companies, ensuring access to vital resources and expertise. In addition, Francis will lead initiatives to strengthen and expand Corundum Neuroscience’s collaborations with key stakeholders, including medtech, medical device, and digital health companies, as well as research institutions and industry leaders worldwide.
“Corundum Neuroscience is at the forefront of advancing neuroscience solutions, and Itsik’s strategic insight and industry expertise will be instrumental in shaping our next phase of growth,” said Yasushi Yamamoto, CEO and Founder of Corundum Corp. “His proven track record in medtech investment and business development makes him a valuable addition to our leadership team as we continue to build and scale transformative neurotechnology ventures.”
Prior to joining Corundum Neuroscience, Francis served as Principal at OurCrowd, where he led key investments and contributed to the launch of the Global Health Equity Fund in partnership with the WHO Foundation. He previously held leadership roles at Medison Pharma Ventures, where he managed strategic alliances and innovation initiatives, and at Ariel Scientific Innovations, where he directed business development efforts. Francis is also the co-founder and former CEO of Citta Pharmaceuticals, a neuro-focused biotech startup. He earned his PhD in Medical Molecular Biology from University College London and conducted postdoctoral research at Columbia University Medical Center, focusing on Alzheimer’s Disease drug discovery.
“I’m excited to join Corundum Neuroscience at such a pivotal time for the neurotech space,” said Itsik Francis. “The CNS vision of translating cutting-edge science into real-world impact resonates deeply with me and I look forward to working with the team to drive new opportunities, strengthen industry collaborations, and support the growth of the firm’s portfolio of ventures.”
This announcement was originally published via PR Newswire on January 28th, 2025. You can view the original release here.
All startups must navigate the “Valley of Death” as they transition from initial discovery and ideation to market launch. This critical period, characterized by heightened risk of failure, is particularly daunting for neuroscience companies, given the complexity of dealing with the human brain and extensive regulatory hurdles involving medical devices.
It is tempting for entrepreneurs, especially those emerging from academia, to focus too narrowly on technological validation. However, deferring crucial factors like regulatory compliance, IP fencing, and market access until later stages of development can prove costly. This is especially true in healthcare, where reimbursement and path-to-patient must be included as part of the early vetting process. After all, there is no point continuing the lengthy development, validation, and verification if the technology does not have the potential to clear all the necessary hurdles.
Here, we examine the key components that neurotech startups must address to traverse the Valley of Death and scale the “Mountain of Opportunity” to commercial success. Addressing these issues up front will provide founders a clear go/no-go on technology development that could otherwise be wasted, enabling you to increase your likelihood of success and realize the full potential of neuroscience innovation.
1. Establishing Clinical Need And Stakeholder Support
A startup must first determine whether its solution addresses an unmet need within the target disease state or positively affects the care continuum, either financially or in terms of outcomes, before establishing a robust scientific foundation. Understanding the fundamentals of the condition, existing treatment options, and patient care pathways is key. But you must also conduct the early market research and stakeholder analysis to confirm your offering is truly novel and offers clear clinical advantages over existing therapies.
The technology must also demonstrate clinical efficacy through early testing and data collection. Without clear proof of concept, you are unlikely to attract investor attention or secure regulatory approval. Incorporating feedback from clinicians, patients, and other users at the earliest stage is crucial. Neurotech companies must therefore integrate a user-centric design process from the beginning, allowing input from providers and patients to shape the final product.
2. Developing Your Approach To Intellectual Property
IP considerations are a key determinant for long-term success and so you must decide early on which avenue to pursue. Following an off-the-shelf strategy will speed up market entry and reduce costs, while also lowering the hurdles for trials and validations. But it will also make it harder to build robust IP. On the other hand, developing something novel from scratch will typically provide a stronger IP position, but it comes with higher costs and longer validation and trial timelines.
You must therefore ensure your technology is defensible, scalable, and able to meet the rigors of the evolving market. By defining your IP strategy and erecting the necessary fences from the outset, you can protect your innovation and competitive edge.
3. Navigating The Regulatory Landscape
Navigating the regulatory environment is one of the most arduous challenges for device makers, with the assigned class determining the level of oversight, trials, and approvals required. Understanding the regulatory landscape early on can smooth the terrain and prevent downstream delays. The opportunity for an investigational device exemption (IDE) or ability to achieve Breakthrough Device designation (BDD) can streamline the approval process and provide unexpected benefits, as when Cala Health secured BDD for its Cala Trio therapy, which saw the company granted two unique HCPCS codes and strengthened its IP.
By building clinical and regulatory teams early on, startups can formulate a coherent regulatory strategy and avoid costly missteps. Understanding the priorities of governing regulatory bodies will create opportunities for you to work with regulators to advance the process. As the regulatory environment evolves, developing a compliance team at this initial stage helps mitigate risks and streamline the approval process, allowing you to focus on scaling the technology.
4. Navigating Reimbursement
Reimbursement is key to financial viability and ultimate success. The technology must appeal to payers by demonstrating cost savings — be it through reducing hospitalization and readmittance, preventing relapses, or lowering the overall cost of care. You must therefore build a strong economic case for your solution and demonstrate early on the ability to reduce the financial burden. You must also address coverage concerns to ensure access to patients. This requires demonstrating clinical effectiveness, cost-savings, and alignment with payer priorities that should be baked into the reimbursement strategy from the outset.
5. Designing For Security And Privacy
Hardware and data security are critical concerns, especially when collecting and transmitting sensitive neural information, as seen with California’s recent passing of legislation to protect consumers’ neural data, following the example set by Colorado earlier this year. Neurotech startups must create a data security plan from the outset, ensuring that all data collection, processing, and storage activities are protected. This must define data ownership, establish clear handling policies, and identify where data is housed.
Key considerations include safeguarding proprietary technology and research with robust security measures across the development cycle, while ensuring third-party compliance among vendors and partners to identify and mitigate potential risks. A thorough risk assessment and developing a threat matrix early on to map out potential vulnerabilities will help secure data flows between all stakeholders and establish a contingency strategy in case of breaches. This will allow you to respond quickly to events and avoid having to retrofit security into an existing system.
6. Strategizing For Market Access And Sales Channels
Having cleared the various development, clinical, regulatory, and financial hurdles, it is essential to have a clear strategy in place for market deployment prior to product launch. You must determine whether to build your own sales network or leverage an existing one that will provide access to the relevant prescribers and physicians. Understanding the concentration and centralization of your customer base will be key to shaping your approach to reaching and engaging potential prescribers.
How the solution is commercialized will ultimately be determined by your target market. Factors including geographic location, accessibility, and the type of healthcare providers involved will further influence sales efforts. Targeting a remote or niche population may require an alternative distribution strategy compared to solutions sold through conventional channels. Tailoring your approach to align with these factors will be crucial to bringing a product to market and ensuring it reaches the intended users.
7. Prioritizing Resources And Expertise
When it comes to tools and resources, integrating all the necessary specialties to get the go/no-go on a technology is something very few startups can accomplish in-house. The regulatory and reimbursement landscapes are especially nuanced, with a single technicality potentially delaying or even terminating product development. Engaging specialist consulting firms that live and breathe regulations and reimbursement can mitigate risks, providing a clearer path to understanding compliance and market access. It also serves to provide that essential interim guidance and support until you are in a position to create in-house clinical and regulatory teams.
Similarly, for engineering and design, instead of building in-house engineering departments, working with specialized firms for the R&D and technological development can shorten timelines and reduce costs. You can then focus internal resources on building a more agile and diverse core team that can handle clinical, regulatory, and market strategies to smooth the path to commercialization.
Scaling The Precipice To Success
The key to surviving the Valley of Death therefore requires a holistic approach from the outset, accounting for all the factors in play – from regulatory hurdles, IP protection, and market access to clinical feedback and reimbursement options. Prioritizing these considerations at the earliest stages of development can provide a clearer path to commercial success, saving valuable time and money in the long run.
Neurotech startups that successfully bridge this valley consider these components early in their journey, allowing them to optimize development strategies and avoid pitfalls. Aligning your technology with market needs, building strong IP portfolios, and anticipating regulatory and reimbursement hurdles, will position you to not only survive the valley but scale the “Mountain of Opportunity” to success.
This article was originally published on MedDevices Online on November 1, 2024, and can be accessed here
Professor Yuval Nir, a renowned sleep researcher at Tel Aviv University, is leading a groundbreaking study to optimize the early detection of dementia and improve outcomes for neurological conditions. Supported by a recent grant from Corundum Neuroscience, his project will investigate a machine learning-based approach to non-invasively detect abnormal brain activity in deep brain regions during sleep.
EEG has been a cornerstone of sleep research for nearly a century, but recent advancements in technology and data analysis are enabling new possibilities. We sat down with Professor Nir to discuss how AI and machine learning are unlocking deeper insights from EEG data, the unique benefits of sleep-state EEG for understanding brain health, and the potential for these advancements to accelerate the diagnosis and treatment of neurological disorders.
Electroencephalographic (EEG) measurements of sleep have been utilized for nearly a century. What recent advancements have been made in this field that change what how it is being used in research and elsewhere?
Prof. Nir: While EEG itself has indeed remained largely the same for nearly a century now, the most significant recent advance in my view is its powerful combination with AI and machine learning. There is much more information in EEG signals than what can be with visual inspection, and AI allows us to extract these signals with great sensitivity. In addition, in terms of hardware, “dry” electrodes (i.e. electrodes that measure the EEG without applying conductive gel) have improved, enabling better quality monitoring in people’ homes – an ambulatory setting – and not only in sleep laboratories.
While traditional research has focused on patterns of brain waves and their functions, your work explores a different type of electrophysiological events. Could you elaborate on paroxysmal discharges, their origins, and what they might signify? Furthermore, how do you interpret their relevance to a broad spectrum of neurological conditions, psychiatric disorders and/or mental health conditions?
Prof. Nir: Sleep EEG includes a number of “signature” brain waves such as slow waves or sleep spindles, which can be seen in all individuals. In contrast, paroxysmal discharges are abnormal brain activity patterns related to excessive, hypersynchronous firing of neurons (i.e. groups of neurons firing together in an abnormally coordinated way). They are most prevalent in epilepsy patients, where they can be associated with seizures, but also occur regularly between seizures as “interictal” activity.
These unique sharp waves are particularly noticeable during sleep and are observed not only in individuals with epilepsy, but also several other neurological disorders such as in neurodegeneration and dementia, in autism and ADHD, and after traumatic brain injury. They often originate from deep brain regions such as the hippocampus and medial temporal lobe, and are therefore difficult to detect with non-invasive EEG. Their relevance lies in their association with cognitive impairment, such as deficits in memory and language, and often suggest a poorer prognosis, for example more rapid cognitive decline in Alzheimer’s disease.
Nearly any neuropsychiatric disorder is associated with abnormal sleep – be it psychiatric disorders such as depression and anxiety or neurological disorders such as epilepsy, Alzheimer’s disease or Parkinson’s disease.
In what ways does sleep-state EEG provide unique insights that cannot be obtained from wake-state EEG? Specifically, how might it elucidate prodromal (early) states of various neurological conditions?
Prof Nir: Sleep serves as a powerful window into how typical and healthy brain activity of an individual is at a given time, both with respect to the general healthy population and also relative to the individual’s usual brain activity. One reason sleep is a good way to gain insight is that when we sleep, our brain goes through stereotypical stages, each with its own signature waves and patterns, making it easier deviations from these patterns. Indeed, nearly any neuropsychiatric disorder is associated with abnormal sleep – be it psychiatric disorders such as depression and anxiety or neurological disorders such as epilepsy, Alzheimer’s disease or Parkinson’s disease.
In addition, beyond sleep being a unique scientific and medical opportunity for monitoring brain health, it also offers technical advantages for better EEG monitoring, as it provides uninterrupted opportunity to record EEG for long hours without eye movements, blinking, and movements that interfere with the clarity of the EEG signal when we are awake.
How do you envision the future integration of sleep technology into daily life? What potential applications and implications arise from the development and widespread availability of accurate, non-invasive sleep monitoring devices for consumer use?
Prof Nir: Ultimately, I imagine that sleep will be monitored routinely at peoples’ homes with touchless monitoring devices that track physiological and brain activities. Combined with AI, it would be possible to construct a model for the typical sleep profile of each individual, and a significant deviation from this pattern would prompt people to consult with their physician for more detailed medical examinations.
Neuralink’s first successful human brain implantation earlier this year brought brain-computer interfaces (BCIs) back into the spotlight, capturing people’s imaginations with the possibilities – and potential pitfalls – of implanting neuromodulation devices into a human brain.
Despite the recent revelation regarding the retraction of some of its connecting threads, Neuralink nevertheless serves as one example of how the neurotechnology industry is advancing solutions that create direct communication pathways with the human brain. A range of factors, including technological breakthroughs, regulatory issues and strategic shifts, have converged to make 2024 the pivotal year for the growth of BCIs.
Pioneering novel materials spurs advancement
A key aspect of the advancement of BCIs will be investigating the incorporation of new materials with enhanced capabilities. One such example is graphene, which presents a promising alternative to silicon-based electrodes due to its superior conductivity, flexibility and charge capacity. It is also considerably thinner than silicon, potentially reducing the pressure on brain tissue and the risk of trauma.
However, being a relatively novel material, it will take significantly longer to navigate the approval processes for its use with implanted medical devices. A champion of the material will need to bear the burden – and cost – of demonstrating its safety and efficacy for chronic implantation. For instance, INBRAIN Neuroelectronics has already secured US Food and Drug Administration (FDA) Breakthrough Device Designation for its graphene-based solution for treating Parkinson’s disease, offering the industry a glimpse of what might be possible when integrating new materials into devices.
Similar pioneering efforts will be needed to prove the suitability of additional emerging materials that will further the use of BCI technologies.
The regulatory landscape: long timelines are essential
At first glance, the regulatory process for neurotech startups appears unnecessarily exhaustive, taking around five-to-six years from the first FDA meeting until a device is granted clearance. However, rather than a bureaucratic obstacle, this is essential to ensure the safety and efficacy of emergent BCI technologies.
The last thing anyone wants is for a therapy or drug to get to market, only to be pulled due to lack of efficacy – or worse, potential danger to patients. This is especially true for the neurotechnology space. So, while the old mantra to “move fast and break things”may have worked in the traditional tech space, when dealing with the human brain it is essential to be intentional and cautious.
The recent Neuralink revelation has highlighted the need for rigorous approvals to ensure the efficacy of new technologies, but this should not detract from the long-term expectations for BCI adoption. It should be emphasized that this was an issue of data capture, rather than a safety concern, and the novel thread system is unique to Neuralink’s approach. Other companies are utilizing alternative methods, such as Synchron using an endovascular approach, while Motif Neurotech is pioneering minimally invasive techniques that do not penetrate the dura of the brain.
Nevertheless, the regulatory journey serves as an essential gatekeeper that, while time-consuming, is essential to establish the foundational groundwork for safe and effective deployment that will pave the path to widespread adoption.
Collaborative regulation helps expedite approvals
While lengthy approval processes must remain, regulators are taking a more collaborative approach towards innovation. Last year (2023), the FDA launched its Total Product Life Cycle Advisory Program (TAP) to facilitate faster development and deployment of safe and effective medical devices. This is achieved by fostering closer relationships between the regulatory body and developers that have demonstrated strong safety and efficacy in conjunction with novel or superior approaches. In October 2023, the FDA announced the expansion of the TAP pilot to include devices reviewed in the Office of Neurological and Physical Medicine Devices.
This more collaborative approach to oversight, moving away from the perceived adversarial relationships of the past towards strategic partnerships with innovative companies, will help accelerate the pace of innovation and expedite some approval timelines while maintaining the necessarily rigorous standards of safety and efficacy. In the end, patients will win.
Joint development of wearable and implanted solutions maintains momentum
While waiting for the longer approval times for implanted neural technologies, increased investment in non-invasive (wearable) BCI solutions will propel the market forward. These solutions are primarily based on electroencephalograms, ultrasounds and magnetic stimulation, such as Magnus Medical, which uses transcranial magnetic stimulation to affect the neural circuits involved in major depressive disorder.
Wearable devices, providing non-invasive brain interfacing, will see earlier and perhaps wider adoption. However, their inability to penetrate deeper into the brain will mean they can only access top-level neural signals, limiting their depth of insight and neuromodulation capabilities.
As such, implanted devices – without the skull as a barrier – will be required to penetrate deeper into the brain to access and transmit neural data with greater depth and specificity. While being invasive may pose greater procedural risks and regulatory hurdles, implanted BCIs will eventually be able to reach deeper and access the cerebral sulci to address a greater number of disease states.
In the continuum of BCI development, wearables and implanted solutions represent complementary approaches to the same goals of greater efficacy, accessibility, and ultimately patient benefit. We are seeing this with companies such as ONWARD Medical running simultaneous external and implantable development programs.
Overcoming the challenge of demonstrating long-term efficacy
As the technology continues to advance, demonstrating solutions’ long-term efficacy represents a key challenge, as BCI devices must be implanted in people’s brains for 5–10 years to establish their safety, which cannot be artificially accelerated.
Given the complexities involved with neuromodulation, it can be tempting to hold devices to a higher standard. While understandable, we should not impose excessive requirements, which are not required by alternative solutions and may hold back the commercialization of these technologies.
This is especially true for cases where devices have the potential to become first-line care, such as with spinal cord injuries or neuropsychiatric disorders. Some models can validate devices for chronic implementation by simulating the body’s response over time, and standards for certificating devices are already stringent. While these should be maintained to establish efficacy and minimize risk, we should not look to establish new performance standards that exceed requirements and stymie innovation.
Continually pushing the boundaries of science and creating stronger starting positions following each discovery will help to propel the industry. Every new iteration, research or commercial project, will allow the industry to learn more and progress. This could help to further shorten timeframes, while working within existing safety protocols.
A point of ethics
As BCI-focused innovation reaches a tipping point, the rapid pace of innovation must be tempered by a commitment to ethical principles. Issues relating to privacy, consent and societal impact all demand careful consideration. This is our one chance to get it right and, dealing with the human brain and people’s neurological wellbeing, we must ensure we proceed in an ethically sound way.
Prudens qui patiens – the prudent man is patient.
We have the opportunity to learn from past endeavors and proceed guided by ethical principles that can best serve all people. If that means going slower to do it, whether through regulatory oversight or strict adherence to ethics, it is the right thing to do.
This article was originally published in Technology Networks on July 11, 2024.
At Corundum Neuroscience, we believe philanthropy can be an instrumental funding vehicle for many neuroscience researchers and entrepreneurs pursuing uncharted areas of science innovation. This brief highlights the imperative role of philanthropy in science, maps out the nonprofit neuroscience funding landscape, and explores emerging funding trends and priorities. In doing so, we aim to illustrate to entrepreneurs and researchers the active role that philanthropy serves in advancing neuroscience research and innovation.
Philanthropy for Science
For over a century, philanthropic funding has played a prominent role in shaping the trajectory of scientific discovery. Alongside government funding, major individual donors and non-profit organizations (NPOs) have served as vital complementary partners, fueling research across diverse fields. A 2022 study reveals the impressive scale of this involvement: US NPOs dedicated a consistent $30 billion annually to science between 2010-2019. This stands in contrast to the National Institutes of Health (NIH) FY2024 budget of $46 billion, of which $3.8 billion is allocated to Alzheimer’s and dementia research.
As federal funding struggles to keep pace with inflation and looming concerns about low grant success rates at federal science agencies, philanthropy is likely to play an increasing role in bridging the gap and ensuring continued progress in scientific research.
A Flexible Partner for Scientific Innovation
Unlike their federal agency counterparts – often constrained by bureaucracy and short-term priorities – philanthropists thrive on flexibility, risk tolerance, and long-term vision. These unique set of traits allows philanthropists to play an outsized role in propelling scientific advancements in various key ways.
First, unburdened by the need for immediate results, philanthropists can provide crucial long-term funding, enabling scientists to pursue ambitious, potentially groundbreaking research that might not fit traditional grant timelines. Philanthropists also often direct funds towards basic science, an area that may face limited government support, and in some cases help institutions acquire expensive equipment that falls outside the scope of government grants. Finally, philanthropists can act as early investors, de-risking promising projects by validating their potential and paving the way for larger government grants later.
Take for instance, the Vera C. Rubin Observatory in Chile; philanthropists assumed the risk of funding the development of a new mirror technology before the National Science Foundation (NSF) provided support. Such funding gaps illustrate the ways that philanthropists work to nurture and sustain an infrastructure that is both resilient and flexible for advancing science.

Philanthropy Ecosystem Supporting Neuroscience and Brain Health
The philanthropic landscape is notably heterogeneous and distributed, where a few large individual donors coexist with many small private funders. Funders with a primary focus on science together account for 93% of all scientific philanthropy. In the neurosciences, the philanthropic landscape is comprised of individual donors, NPOs – which includes private foundations, family foundations, community foundations, public charities, and corporate funders. Funding for neuroscience research relies disproportionately on individual donors, whose contributions often take the form of endowed or expendable gifts to universities or research institutes. While quantifying individual contributions can be challenging, a 2020-2021 analysis by the Chronicle of Philanthropy’s Big Gift Database identified $600 million for the construction of research facilities within neuroscience and neurology.
NPO and corporate funders are playing a smaller yet meaningful role in advancing neuroscience research by filling the gaps left by federal funding. A key example is the directed-use grant model, where philanthropists contribute to specific projects aligned with their interest. This approach accounted for a significant $4 billion (or 8%) of basic-science funding at universities and research institutes in 2016 alone.
In 2022, Stanford University announced a $75 million gift from the co-founder of Nike to establish the Phil and Penny Knight Initiative for Brain Resilience. Driven by the initiative to combat neurodegeneration, they will establish the Brain Resilience Laboratory as well as funding for innovation grants and postdoctoral scholars. Considering the varying interests and goals of NPOs supporting neuroscience, Inside Philanthropy’s 2023 report on Neuroscience Research identified the following subsets of funder types:

Funding Trends
Neuroscience research faces growing challenges. Declining grant acceptance rates are siphoning crucial resources, while top scientists are dedicating a staggering two-fifths of their time on activities outside of research such as looking for funding.
In response, philanthropists are emerging as champions of innovation, not simply by refining established funding methods, but by forging creative pathways to bolster resources, expand their reach, and ultimately, accelerate scientific progress. This shift has helped to facilitate a more supportive environment for neuroscience researchers and entrepreneurs, as evidenced by the following trends:
Rise of Nonprofit Venture Philanthropy
Philanthropists are venturing beyond traditional grant-funding by diversifying their impact strategies. A growing number are creating mission-related investment funds that blend elements of venture capital (VC) and nonprofit structures. These funds, sometimes referred to as “venture philanthropy,” operate as nonprofits managed by philanthropic sponsors but raise capital through donations. This unique approach empowers donors to directly influence investment decisions and ensure that any returns generated are reinvested for further impact, unlike traditional VC where profits go back to investors.
Venture Philanthropy offers several advantages:
Direct Impact: Donors have a greater say in how their contributions are used and can target them towards specific research areas or companies.
Higher Risk Tolerance: Unlike traditional grants, these funds can invest in riskier but potentially groundbreaking research that might struggle to secure funding elsewhere.
Sustainability: Reinvesting returns creates a perpetual funding source, amplifying the initial investment’s impact over time.
The potential of this model is exemplified by the Alzheimer’s Drug Discovery Foundation (ADDF), which has funded over 50 neuroscience companies in the past decade, both by awarding grants and participating in late stage funding rounds. “As a venture philanthropy, the ADDF seeks out and invests in the most promising, high-risk/high-reward science from biotech companies and academia that would go underfunded without us,” explains Chief Philanthropy Officer Jane McIntosh.
Underscoring this growing trend, the table below showcases non-drug neuroscience companies that have received funding from nonprofit VCs in recent years.
Linking Avenues for Collaboration
Recognizing the inherent complexity of neuroscience research, funders are increasingly embracing powerful partnerships like the US Brain Initiative to achieve meaningful advancements.
Collaborative funding seeks to break down silos and foster joint efforts across diverse stakeholders, including foundations, government agencies, academic institutions, industry leaders, venture capitalists, and philanthropic organizations.
Below are a few notable examples of collaborative funding in the neuroscience domain:
Breaking Silos | One major hurdle in research progress is the fragmented nature of funding across different entities. To tackle this challenge, the Research Corporation for Science Advancement (RCSA) took the initiative to coordinate collaborative funding opportunities for both new and established science philanthropists, fostering collaboration among organizations like the Heising-Simons Foundation, the Paul G. Allen Frontiers Group, the Chan Zuckerberg Initiative, and the Sloan Foundation.
Accelerating Diagnostics | In the area of Alzheimer’s and dementia research, the Alzheimer’s Drug Discovery Foundation (ADDF), co-founded by prominent figures like Leonard A. Lauder, Bill Gates, Jeff Bezos, and the Dolby Family, launched the Diagnostics Accelerator with the aim to find and fund bold ideas for easier, more accurate, and earlier diagnosis of these diseases. This initiative, with a total commitment of $100 million since 2018, has garnered additional support from diverse partners like the NFL Players Association, Eli Lilly & Company, Biogen, and the Shanahan Family Foundation, highlighting the power of collective action.
Brain Health Research | Launched in May 2021 at the World Economic Forum, The Health Brains Global Initiative (HBGI) is a $10 billion initiative to advance brain science breakthroughs. HBGI received initial funding and support from OneMind, the National Academy of Medicine, Johnson & Johnson, Otsuka and the Wellcome Trust.
Philanthropy Spinoffs – Focused Research Organizations
Traditional grant-funding for scientific research is seeing a transformation with the emergence of focused research organizations (FROs). FROs offer a unique alternative, allowing NPOs to directly invest and guide the direction of niche projects that might otherwise struggle to secure funding or languish on an idea shelf.
Unlike traditional avenues like academic labs, which might perceive some projects as too risky or complex, or industry/VC, where profitability takes precedence, FROs provide a vital lifeline. They can support projects like the one undertaken by E11 Bio, which aims to map the complex neural circuitry of the brain, a feat requiring experts who wouldn’t necessarily find suitable opportunities in traditional settings.
The potential of this model is evident in the joint $70 million commitment by the Astera Institute and the Buck Institute for Research on Aging to support an FRO studying longevity. Such collaborations unlock doors for groundbreaking research that holds immense promise for various fields.
Diversity, Equity, and Inclusion
As our population ages, concerns are intensifying around how neurological conditions disproportionately impact specific ethnic and racial groups. In response, funders are increasingly making diversity, equity, and inclusion (DEI) an important tenet of their grantmaking strategies. This shift aims to address representation gaps in clinical trials, understand the socioeconomic factors influencing health disparities, and embed equity within research organizations.
Key Focus Areas Include:
- Boosting Diversity in Clinical Trials: Initiatives like The Parkinson’s Foundation’s $10 million investment in 2021 actively recruit underrepresented minorities for crucial research.
- Examining Social Determinants of Health: Funders like The Sloan Foundation require grant proposals to address how research projects will promote broader participation, acknowledging the impact of social and economic factors on health outcomes.
- Promoting Equity Within Organizations: The overall goal is to foster more equitable and inclusive research environments across the board.
Such steps mark a crucial shift in acknowledging the disparities faced by specific groups and driving a more inclusive approach to neurological research.
Interdisciplinary Research
Funders are recognizing the immense potential of interdisciplinary research, viewing it as a fertile ground for uncovering unexpected discoveries and breakthroughs. In neuroscience, research into the underlying complexity of the brain often yields findings that can be applied to disorders associated with mental health.
“There’s a lot of interconnectedness and comorbidities, and when you fund this kind of research, you sometimes get findings that you didn’t expect,
Beth Lewin Dean, CEO, CURE Epilepsy
Organizations like The Kavli Foundation support research institutes exploring intersections between seemingly unrelated fields like astrophysics, theoretical physics, neuroscience, and nanoscience. By employing advanced computational, imaging, and visualization techniques across disciplines, interdisciplinary research collaborations aim to uncover previously unimaginable discoveries.
Crowdfunding
Crowdfunding, often referred to as “citizen science” in research contexts, has emerged as a novel funding method for researchers and entrepreneurs. While individual contributions might be smaller compared to traditional grants, these platforms have democratized access to funding, opening doors for innovative projects regardless of background or affiliation.
Several prominent philanthropic organizations, including the Simons Foundation, Schmidt Futures, and the Burroughs Wellcome Fund, have recognized and supported this trend. For instance, the Sloan Foundation directly funded the development of influential citizen science platforms like Zooniverse and SciStarter. Notably, crowdfunding is also gaining traction as a strategy for corporate philanthropy, enabling wider participation in supporting non-profit initiatives. A study titled “America’s Charity Checkout Champions” found that charity campaigns raised over $486 million in 2018 alone.
— —
Philanthropy in the life-sciences, particularly within neuroscience, can play a small but vital role in advancing innovative research and funding emerging companies. With an annual commitment of $30 billion in the United States alone, philanthropic support offers flexibility, risk tolerance, and long-term commitment for ambitious ideas that often require longer-innovation cycles, filling gaps left by traditional grant structures and venture capital investment.
Furthermore, the emergence of novel funding models, such as nonprofit venture philanthropy and focused research organizations, underscores a growing commitment among philanthropists to address complex challenges and explore untapped avenues of inquiry while supporting emerging companies in neuroscience and related fields. For researchers and entrepreneurs in this domain – understanding these diverse funding environments can ensure you capitalize on available opportunities and secure the necessary support for your innovation.
References
- https://www.insidephilanthropy.com/state-of-american-philanthropy-pdfs/giving-for-neuroscience-research
- https://www.nature.com/articles/d41586-023-00077-2
- https://www.the-scientist.com/careers/philanthropic-funding-makes-waves-in-basic-science-30184
- https://pubs.aip.org/physicstoday/article/71/6/26/803564/Foundations-play-a-supporting-role-in-basic
- https://issues.org/envisioning-science-unknown-future-philanthropy-cordova/
- https://www.science.org/doi/10.1126/science.abq2259
- https://www.philanthropyroundtable.org/magazine/the-power-of-science-philanthropy/
- https://sciencephilanthropyalliance.org/philanthropy-a-critical-player-in-supporting-scientific-research-alliance-blog/
- https://news.stanford.edu/2022/04/26/stanford-knight-initiative-brain-resilience-will-combat-neurodegeneration/
- https://www.economist.com/leaders/2023/11/16/to-supercharge-science-first-experiment-with-how-it-is-funded
- https://www.palmbeachpost.com/story/news/2020/03/21/startups-offer-promise-for-alzheimerrsquos-cure/112263954/
- https://www.axios.com/newsletters/axios-pro-rata-0ce2c100-f3af-440f-8864-7064ada698a7.html?
- CNS Pitchbook Search, 2023.
- https://www.braininitiative.org/mission/
- https://philanthropynewsdigest.org/news/healthy-brains-global-initiative-to-raise-10-billion
- https://www.philanthropy.com/article/quick-grants-from-tech-billionaires-aim-to-speed-up-science-research-but-not-all-scientists-approve
- https://issues.org/future-science-philanthropy-sloan-michelson-falk/
- https://issues.org/tag/sloan-foundation/
Over recent decades, neuroscience has transitioned from a predominantly academic endeavor to a field rich with commercial potential. Consumer neurotechnologies emerged in the early 2000s with NeuroSky’s EEG-based toys, which decoded brain waves to move objects. In the burgeoning landscape of technological innovation since then, neuroscience startups have promised breakthroughs ranging from enhanced brain-machine interfaces to novel therapies for neuropsychiatric conditions. Yet, a sobering pattern has emerged as, too often, these startups find themselves struggling early on, or worse, declaring bankruptcy.
This can, and has, damaged the reputation of the domain, with nightmarish consequences. Up-and-coming solutions produced by companies in the field can suffer from years of setbacks to their progress, as financial resources and talent flock to other, more lucrative sectors. Moreover, the regulatory and reimbursement bodies may become more stringent in their standards, while consumers may dismiss rigorous reproducible neuroscience research with blanket statements.
Such events send shockwaves through the investor community. Due diligence processes become more invasive and capital scarcer, even for promising startups in the same vertical, sowing investor doubt in the broader neuroscience startup space. This can lead to reduced funding for an extended period, stifling innovation and growth and resulting in slower growth until the sector can achieve both the technological maturity and venture confidence needed to build and commercialize in the space.
While conventional wisdom emphasizes the significance of product-market fit and founder fit, we have seen that the downfall of neuroscience startups often arises from complex factors that are regulatory, financial, and clinical in nature.
With the tremendous impact that neuroscience innovation is poised to have on humanity, founders and investors have an opportunity.
By understanding the traps and challenges — seeing where others have failed — entrepreneurs in this sector can map their strategies early on, address these issues, and set themselves up for long-term commercial success.
1. Regulatory Barriers to Neuroscience Advancement
The stringent FDA regulations for medical devices and therapies demand rigorous testing and evidence of efficacy. Companies such as neuromodulation startup Nuvectra had promising technologies, but still filed for bankruptcy due to regulatory hurdles that prolonged their product’s time to market. Even if a startup can survive the prolonged development phase, the cost involved in regulatory compliance is often exorbitant, putting immense financial strain on the organization.
Some neuroscience solutions have been reclassified by regulatory agencies over the years. For instance, Nixon’s War on Drugs has prevented the use and research of many psychedelic substances in the United States since the 1970s. However, in recent years, academic research has demonstrated the safety and efficacy of psychedelic substances in improving outcomes for various mental health conditions. As a result, some types of psychedelics have become decriminalized in a select few states. With a growing pool of trained psychedelic practitioners, psychedelics are only now becoming a more accepted treatment option.
On the flip side, some well-researched devices with strong safety profiles are facing tighter regulations. In 2022, EU regulators reclassified noninvasive brain stimulation devices not intended for medical purposes as Class III medical devices. This resulted in technologies such as transcranial magnetic stimulation and transcranial electric stimulation, which optimize brain activity without surgery, being regulated as strictly as technologies that require surgical implants in the EU.
We’ve seen legislation in the neuroscience space shift over time, with the changing culture and scientific understanding of decision makers. This has posed a barrier for many in the space to advance from research to commercialization.
Keeping an eye on the regulatory landscape, understanding its direction, and working with advocacy groups to steer it forward can help founders navigate the regulatory minefield and ensure they are working in an environment that can support the adoption of new neuroscience solutions.
2. Reimbursement Models Prevent Market Entry
Startups in the neuroscience space must also navigate the intricacies of healthcare reimbursement models. Unlike tech companies where revenue often starts flowing soon after market entry, medical technologies often face long gestation periods before they are covered by insurance, a pivotal factor in consumer adoption.
Pear Therapeutics serves as a compelling example of the challenges that neuroscience and digital therapeutics startups face. The company had secured FDA approval for its prescription digital therapies, suggesting a strong product-market fit. Yet, Pear Therapeutics struggled with insurance reimbursement and had discrepancies in its clinical trials, which evaluated a different product than that which it was trying to commercialize. This led to bankruptcy and caused investment in the digital therapeutics sector generally to dry up.
Interestingly, some neuroscience wellness products are neither reimbursable by insurance or tax-advantaged accounts but have nevertheless achieved strong market penetration and helped many people to be proactive with their health. This has been the case for wearables, meditation aids, and monitors for sleep and exercise. However, companies developing wellness products face the challenge of creating moats of defensibility in a world of potential copycats, as well as true demonstrations that the products do what they claim to do. These defenses can come through intellectual property strategy and a strong applied science backbone for the technology.
Notwithstanding, learning from the Pear Therapeutics example, neuroscience solutions must have strong product-market fit, the science must fully back up any claims for the specific product in question (more on this next), and there must be a pathway to reimbursement from the healthcare system.
3. Scientific And Clinical Evidence Can Make Or Break A Startup’s Success
Rigor and reproducibility in science are critical elements for a company’s success. A startup’s leadership must therefore ensure they fully understand how to evaluate scientific research and assess risks. If not, they may find themselves hamstrung in reproducing results with their products.
The scientific rigor required to substantiate medical claims is exceptionally high. And while science serves as the foundation of engineering, if engineers ignore the science when building, they may end up creating a “pseudo technology” that claims to do something it cannot.
To overcome the hurdles of rigor and reproducibility of neuroscience technologies, founders must provide robust scientific and clinical evidence in well-controlled studies and with well-constructed technologies. In doing so, they can win the trust of consumers and medical professionals.
Despite the immense potential to improve lives, neuroscience-based technologies, such as transcranial magnetic stimulation devices, often require specialized training to be used properly. Relatively few psychiatrists are neuropsychiatrists. Among those early adopters of new neuromodulation devices, the training timeline can have a limiting effect on the adoption of the technology, even if the clinical outcomes demonstrate great safety and efficacy. Similarly, mental health treatments using ketamine and psychedelics may need specialized training among clinicians to aid patients in their healing journey. These market dynamics make it difficult for solutions to reach patients.
4. Consumer Acceptance Beyond Early Adopters
As such, some startups begin, pivot, or expand into wellness products to circumvent stringent medical regulations. Wellness devices are not required to have their claims evaluated by regulatory agencies, such as the FDA, but may have the potential to improve people’s lives. However, moving to non-medical status requires a change in marketing focus, from clinicians to a wider consumer audience, necessitating a shift in strategy and customer engagement models — something companies may not be prepared for.
Whether for medical use or wellness applications, there remains intrigue among consumers and clinicians in the possibilities created with neuroscience-driven innovation. Yet, transitioning from early to mass adoption still poses a significant hurdle. Technologists, entrepreneurs, neuroscientists, and others invested in developing these new technological approaches must carefully consider their goals, who their end users are, and the financial runway that will be required long-term to achieve market acceptance.
Implications And Forward Outlook
The issues at hand are neither superficial nor easily navigable. Failure to address the issues will stifle innovation and jeopardize the substantial investments made in this sector. These are systemic hurdles that can obstruct even the greatest neuroscience startup teams.
Yet, knowing about the issues contributing to the failure of previous neuroscience startups can facilitate the development of resilient business models and help realize the sector’s immense promise. We can see the unique challenges in this space, and we are excited to develop robust strategies that extend beyond conventional notions of product and founder fit.
Collaboration between startups, regulatory agencies, and reimbursement authorities can pave the way for effective solutions. By understanding these common problems and proactively adopting strategies to mitigate them, startups in this field can navigate the complexities with greater confidence and integrity, and ultimately position themselves for long-term success.
Article originally published in Med Device Online
About The Authors:
Liron Nunez Weissman is the CEO of Corundum Neuroscience, a venture builder and fund advancing transformative neuroscience solutions from lab-to-life.
Sharena Rice, Ph.D., is a research scientist at Sanmai Technologies PBC and a contributing editor at Neurotech Reports.
For centuries, humans have been fascinated by sleep, and our understanding of it has traced an arc from mythic to scientific. In the early 20th century, the advent of electrophysiological recordings measuring brain activity provided a significant boost to sleep and dream research.
These discoveries opened the door for the investigation of the links between sleep and health, and led to the development of new technologies for diagnosing and treating sleep disorders.
Fast forward to today, as global sleep awareness grows, the need and demand for effective sleep innovation is more acute than ever.
Sleep Loss Epidemic by the Numbers

Sleep has become a critical market precisely because a society without rest pays a premium. Workplace absences, a decline in productivity,
and an increase in healthcare expenses due to sleep- deprivation-related maladies can cost companies—and countries—billions.
Capital Investment and Deals in the Sleep Tech Market
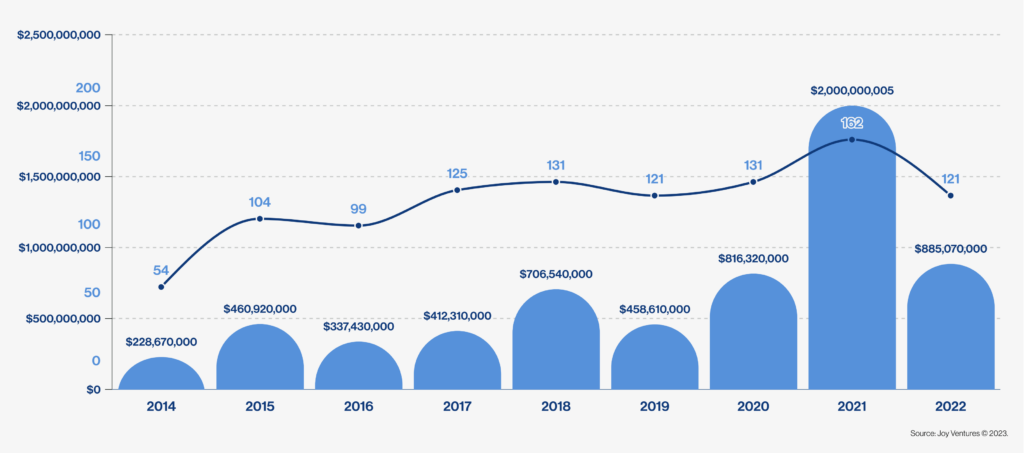
Venture capital investment has steadily increased to a total of +$5B over the past decade, with an upsurge following COVID-19 pandemic-induced sleep disturbances.
Despite capital market slowdowns in 2022 in response to the interest rate environment, Joy’s internal research of 450 sleep-tech companies indicates a strong investment appetite in the sleep-tech market.
Available Sleep Technologies on the Market

The global sleep tech devices market size was valued at USD15,407 Million in 2021 and is estimated to reach the value of USD 60,955 Million by 2030, growing at a CAGR of 16.8% from 2022 to 2030.
As the next era of sleep science and innovation ushers in, this brief offers a glimpse into the future and includes insights on topics such as:
- The current state of the sleep economy
- Investors’ appetite for available sleep technologies and their respective revenue potential
- Perspective from leading neuroscientists on advancements and future trends in sleep and circadian rhythm innovation
- Two research angles that we believe are ripe for exploration:
1. Sleep and Wake Optimization
2. Sleep as Data
Sara Shnider, our US Academic Innovation Lead, discusses how advancements in brain imaging, genetics, neural stem cell models, and AI are enabling groundbreaking personalized health interventions, bridging the gap between neuroscience research and real-world solutions, and her approach to collaborating with academic scientists to translate their breakthrough discoveries into impactful applications.
What excites you most about driving academic innovation in neuroscience, and how do you see CNS contributing to this effort?
Over the last decade, there has been tremendous scientific and technological progress in the neurosciences. Breakthroughs in genetics, advances in human stem cell models, and sophisticated technologies for monitoring brain activity, combined with integration of artificial intelligence (AI) approaches for data analysis, have moved us into a new era of deciphering this fascinating and complex organ that is the brain. Looking into the future, I am excited by all the possibilities of translating these scientific advances into new and effective solutions to treat devastating diseases and injuries to the nervous system.
I find it highly motivating to collaborate with academic scientists on transforming their cutting-edge discoveries into applications that can improve human health. Their creativity and scientific rigor as they push the boundaries of human knowledge is inspiring. However, the incentives in academia typically prioritize publication over commercialization and entrepreneurship, and there is a need to identify those high potential projects that with financial investment and mentorship can be developed into commercially viable products to benefit society.
CNS is contributing by taking a multi-pronged approach toward driving academic innovation by funding research, building companies, and investing in startup companies in the neurosciences. In some cases, CNS funds research within academia to help advance and mature technologies toward commercialization. In other cases, there is existing intellectual property (IP) available for licensing and CNS helps with incubating the companies as they develop their product and business plan, and provides support with strategic advisors and funding. CNS also has a more traditional VC role in funding early stage startup companies from pre-seed to Series A. By combining these approaches, CNS takes the long view and can also invest in efforts that need further research.
In your opinion, what are some of the biggest challenges and opportunities facing neuroscience today, and how can we work together to overcome them?
One of the greatest challenges in drug development for neurological disorders is patient heterogeneity. Patients are diagnosed into distinct disease classes, but in practice patient symptoms and disease progression are often highly variable. This makes it challenging not only to design clinical trials, but also to know which patients will respond to which intervention. In psychiatry in particular, finding the effective treatment typically involves a lengthy process of trial-and-error that prolongs patient suffering and increases costs. There is a recognized need to shift toward more nuanced biomarkers for diagnosing and subtyping patients based on disease mechanisms to enable development of personalized treatments. This is a transformation that the field of cancer therapeutics has undergone over the last 20 years, where treatments are now being tailored for each patient based on the genetic profiles of the tumor.
That being said, this is also an era of remarkable progress in genetics, brain imaging, and neural stem cell models derived from individual patients. When these tools are combined with powerful artificial intelligence approaches, it enables patient classification based on underlying disease mechanisms and brain circuitry, and opens the door to development of personalized interventions. One exciting example in the neurodegenerative disease space is the recent FDA approval of a drug to treat a genetically defined subset of people with amyotrophic lateral sclerosis. There are also exciting efforts in personalized psychiatry, using patient-derived stem cells and AI to predict which treatment will be most effective for each patient.
One avenue where I think the clinical and research communities could work together is to increase reporting of unsuccessful research studies and clinical trials. There is a need to incentivize sharing and publication of negative results, so that the stakeholders involved in developing new neuroscience solutions could learn from each others’ experiences and move faster toward successful results.
Another challenge has been the lack of representation of diverse populations in clinical research, albeit this is not a challenge unique to the neurosciences. According to data from the Food and Drug Administration, in 2020 75% of clinical trial participants were white, and the majority of clinical trial volunteers have historically been male. There is a need for more inclusive clinical studies to include more women, racial and ethnic minorities, and participants from diverse geographic and socio-economic backgrounds. In addition to being an ethical issue about health equity, diversity of clinical research participants is essential to determine safety and efficacy of therapeutic interventions across different populations. On this front, the boost toward remote clinical trials that occurred during the COVID-19 pandemic has created a new opportunity for inclusivity. Leveraging wearables, sensors, and telehealth, it is now increasingly possible to broaden the participant population to include people who may not have easy access to clinical trial sites. Social media also provides an opportunity to increase patient engagement and access diverse communities for clinical trial recruitment. But of course, it is a gradual process and there is still so much more progress needed in this direction.
What made you want to pursue a career in life sciences, and how has your background prepared you for your role at CNS?
At this point it may be cliché’, but my interest in neurosciences started when I read “An Anthropologist on Mars” by the late Dr. Oliver Sacks. In The Case of the Colorblind Painter, he tells the touching story of an artist who needs to re-invent their identity at age sixty-five following a concussion that leaves them colorblind. I became fascinated by the complexity and mystery of the brain. Although it appears to be just another multicellular organ in our body, it is intricately tied to our identity, and when injury or illness disrupts brain function, it changes our personality and sense of self. I decided to pursue an undergraduate degree in biology with a focus on neuroscience, and a PhD in neurobiology. My research focused on elucidating how diverse neurons in the neocortex, the brain region responsible for most high-level cognitive functions, acquire their identity and specialized function during development.
Over the last 10+ years since graduating from my PhD, I have focused on translating innovative scientific discoveries into applications that can benefit patients through industry-academia partnerships. I have worked at both a large academic medical center and a global pharmaceutical company on strategic and operational aspects of collaborative research projects, as well as licensing and entrepreneurship programs. I look forward to leveraging this expertise to lead CNS’s efforts to develop new health solutions in the neurosciences by building a diverse portfolio of partnerships with academic investigators in the United States.
What strategies do you find most effective for driving progress in academic innovation (particularly in terms of translating research discoveries into real-world solutions)?
I believe that it is extremely valuable to have partnerships with stakeholders outside academia that intend to use and/or commercialize the technology. Having this perspective incorporated into the scientific direction early on can substantially accelerate progress toward commercialization of academic innovations. However, there is no ‘one-size-fits-all’ approach that works for situations. For some early stage projects with commercial potential, the most effective approach may be a short-term pilot grant to explore a novel approach, while a technology that is more developed but that requires further validation may best be served through a multi-year collaborative research project that includes a licensing agreement with a strategic investor. For some innovative projects, an incubator for launching a startup company might be the best launchpad.
That being said, there are some critical elements for successful commercialization of academic innovation. The partnerships need to be mutually beneficial. For example, academic investigators need to publish, while industry partners put a premium on confidentiality and profits. For successful research collaborations, all parties need to understand the incentives and objectives of their partners and yet still feel confident that their interests are being addressed. In addition, as in any team effort, the relationships are key. It is essential to have a perspective of building long term relationships and prioritize establishing trust between the partners. As relationships become more established, everyone becomes more invested in the project’s success.
Looking ahead to the future of neuroscience research, what do you think will be some of the most exciting developments in the field, and how can we ensure that these advances are used to benefit society?
There are some very exciting advances in technologies for imaging, tracking and modulating brain activity. One example is novel non-invasive neurostimulation approaches to alleviate severe depression in people who have tried multiple pharmacological interventions with no success. Over the next decade, I would hope to see a breakdown of the silos the pharmaceutical and medical device industries, and new solutions involving both drugs and devices that may in combination work better than either approach alone.
Another exciting area that is progressing rapidly is the field of brain-computer interface (BCI) technology, where a device records and analyzes brain activity and decodes it to control a robot or send commands to a computer. These technologies open a whole world of potential for people with limited mobility or loss of speech, such as in ALS. These BCI solutions are continuously improving, and I look forward to seeing how they are applied to increasingly help patients overcome disabilities due to injury or disease.
I believe investors play a meaningful role in steering scientific advances toward societal benefit. It is exciting to be part of a team that is driven by turning scientific discoveries into products that solve unmet needs in the neurosciences. I look forward to sharing more about our activities as we move forward with new projects and investments!
When we crave a snack, why do we often find ourselves reaching for that cookie instead of an apple? Clearly, one option is healthier than the other, and yet our temptations override our better judgment. How can we break out of that cycle to make better life choices? Is there a way to overcome behaviors like biting our nails when we get nervous or downing that bag of chips when our stress levels start to peak?
Our most recent grantees are an interdisciplinary team of researchers at the University of Haifa currently working to empower people to overcome their hard-to-break ingrained habits by using non-invasive brain stimulation to shift their behavior towards more beneficial life choices and behaviors. The team includes Dr. Shai Gabay, associate professor at the evolutionary cognitive neuroscience lab and the head of the Institute of Information processing and decision making (IIPDM); Dr. Yafit Gabay senior lecturer at the learning and language lab and Dr. Uri Hertz, senior lecturer at the social decision-making lab. They will explore how transcranial direct current stimulation (tDCS), a painless solution that uses electrical currents to stimulate specific parts of the brain, can activate the neural centers that directly control attention and eye movement, which are associated with attention and decision making.
tDCS is a brain stimulation method that can be applied to modulate areas in the brain associated with addictive behavior and drug abuse. It is also used for many non-medical wellness applications such as accelerated learning, focus, relaxation, and meditation.
Using this method together with activating participants’ frontal eye field (FEF), a part of the brain responsible for saccadic eye movements (rapid, ballistic movements of the eyes that abruptly change the point of fixation) and attentional orienting, they hope to influence participants’ choices and steer them away from their current habits by modifying their ‘free will’” by activating neural mechanisms that will produce an artificial attentional bias without them being aware of this taking place in their brains.
Why this is different and how they’re doing it:
Until this point, previous studies focused on manipulating neural regions of the brain involved in decision making and control. This approach will bypass these processes and influence behavior by activating the brain’s neural centers that directly control attention and eye movement which is known to have an effect on people’s behavior patterns, and in this case, their ‘bad habits.’
The research team is expanding on the latest developments in the computational modeling of decision making and attention. The lab work will start by examining whether tDCS can be used to influence participants’ choices in a ‘free-will’ task. In the next phase, they will use the same technique to see if participants can overcome habits that are formed within the laboratory setting – shifting choices towards counter-habitual over habitual responses. And finally, they will evaluate whether this can be applied in a real-world situation to be used to overcome actual and harmful habits connected with self-control and attention.
Helping people make better food choices
One of the most promising areas of real-life application of this research is helping those who struggle with habitual external eating, or eating food not only when they are hungry, but just in reaction to sights and smells. But the potential applications are endlessly vast, especially because the therapy should be able to be tailored to treat conditions at different stages, for both long-term and short-term relief.
”Such an approach may be useful in a variety of severity levels, providing a small boost or a longer treatment protocol where needed,” says the researchers. “Our approach may also provide novel scientific insights concerning the neural mechanisms that control the interactions between attention and habit formation, and establish a new experimental procedure to better characterize the neural and cognitive basis of habit formation and deployment.”
Overcoming bad habits can seem almost impossible, especially when they are hard-wired into our brains and seem to control our every behavior. While finding a solution to this age-old problem may seem daunting, this is exactly the thing that inspires us at CNS. We are excited to get in on the ground floor with this cutting-edge research that has the potential to pave a path toward improved wellbeing in a way that can be accessible, consistent and effective.
We all know that a good night’s sleep is essential for a healthy mind and body and that a lack of sleep can lead to various physical and mental ailments, including exhaustion and difficulty concentrating. But lack of sleep can underpin almost all of our daily functions, including our ability to empathize with others.
While not often discussed or studied, empathy is a basic social skill, involving both cognitive and emotional aspects. It alerts us if a person is in pain or distress, and allows us to relate to or care for them accordingly. Not only is empathy important for building healthy relationships, but it is also crucial for many professions, and for a healthy and functioning society.
Our interdisciplinary group of grantees– Alex Gileles-Hillel, a doctor in the pediatric pulmonology and sleep unit at Hadassah Medical Center, Shoham Choshen-Hillel, a Hebrew University business school professor, and Anat Perry, a psychology professor at the Hebrew University– will delve deeper into the connection between sleep and empathy and explore potential remedies to improve healthcare professionals’ wellbeing and job performance.
Addressing an ongoing hidden problem in healthcare
By supporting this new research project in Jerusalem, we hope to advance the understanding of how sleep affects empathy, especially among physicians, who often work long shifts without rest. This sleep deprivation can cause their levels of empathy to drop, decreasing their ability to connect with patients in order to effectively treat them.
This research, which is the first to investigate the direct effects of sleep on empathy, revolves around testing CogNyx, a non-invasive headband developed by our portfolio company, NYX Technologies that helps the wearer achieve the optimal natural brainwave patterns necessary for falling asleep and entering deep sleep, and the effects this device has on improving sleep quality and cognitive and social functioning.
The goal is to change the autonomic nervous system to increase empathy by developing an intervention to reduce the negative effects of doctors’ sleep deprivation on both their ability to be present and compassionate as well as their ability to diagnose and treat their patients.
In addition to measuring sleep quality, our grantees will study its direct link to empathy by examining how participating doctors respond to pain, the emotions of others and overall decision-making ability after sleeping with or without the use of the CogNyx device.
Opening the door to better sleep and empathy for the larger population
The CogNyx device and associated research on the links between sleep and empathy have potential to increase wellbeing for people beyond doctors and their patients, who no doubt benefit from their caregivers’ increased empathy.
Eventually, such a headband or other wearable device could be an effective solution for the mainstream population to enable more people to benefit from better sleep.
“Sleep deprivation is a modern-day epidemic affecting nearly every sector of the population, gaining a better understanding of its effects and how to measure and overcome them, should have immense implications for all parts of society, from insomnia patients to parents of young children to shift-workers and anybody else struggling to get a good night’s rest, ” explains Gileles-Hillel.
We are excited to see where this research will take us and how it can potentially open up more possibilities to solve the problem of sleep deprivation to enable more empathy not just for doctors treating their patients but for all suffering from sleep deprivation.
While sleep disruptions, working long hours and night shifts are things we cannot change, the path towards better sleep and gaining all the benefits from this important life function can be eased through this groundbreaking research. By combining multidisciplinary research and cutting-edge technology, we are sowing the seeds of a more compassionate and better future.
Since the onset of the pandemic, more people have been seeking out alternative methods to reduce stress, anxiety, depression and other mental disorders with meditation as an increasingly popular choice.
With over 35 million adults saying they have tried meditation at least once, the number of people engaging in this practice has tripled since 2012. This increase is also reflected in the meditation & mindfulness industry, now estimated to be worth about $1 billion.
However, many people who try mindful meditation, which requires high levels of discipline and can bring up painful memories, are unable to stick with the practice long enough to reap the benefits that improve depression, anxiety and other conditions.
Our 2020 grantees Dr. Joseph “Jay” Sanguinetti, assistant director of the University of Arizona’s Center for Consciousness Studies, and Prof. John J. B. Allen, Distinguished Professor of Psychology, are developing a non-invasive technique to help people feel the benefits of mindfulness more quickly, and thus stay with the process, creating a cycle of benefits.
Making the most of meditation: Facilitating mindfulness training with ultrasonic waves
By fostering an attitude of acceptance and emotional resilience, mindfulness through meditation has proven effective for many people struggling with mental and emotional disorders such as anxiety and depression. The ancient practice has risen sharply in popularity recently, partly due to the stress of the pandemic, with the number of adults who say they have meditated at least once tripling since 2012. But feeling the benefits of mindfulness also requires a high level of discipline and commitment over many months. It is only with dedicated practice of intense meditation that the brain will enter what experts call a state of equanimity, or acceptance, which is ultimately what improves one’s mood and boosts energy while reducing stress.
Unfortunately, data shows that most people are unable to maintain a regular practice of mindfulness long enough to achieve this equanimity and reap its long-term benefits. Developing the discipline that mindful meditation requires, and sticking with it regularly can be especially challenging for those who need it the most. For example, people with depression can experience a ‘backdraft effect’ where mindful meditation ends up making them feel worse in the short term – triggering past traumas and depressive thoughts, which makes them less likely to stick with the practice for the long term, when it can eventually have a positive effect.
But, what if achieving mindfulness was less of a struggle? What if there were a shortcut to training the brain to benefit from such practice early-on, motivating people who need it the most to commit to a more effective practice? This is exactly what our scientists, Dr. Joseph “Jay” Sanguinetti, assistant director of the University of Arizona’s Center for Consciousness Studies, and Prof. John J. B. Allen, a Distinguished Psychology Professor at the University of Arizona, are working to achieve. Their goal is to harness technology to get more people to equanimity quicker and keep them on the path towards mindfulness long enough to really change their lives and improve wellbeing.
A Modern Day Approach to an Age-Old Practice
Dr. Sanguinetti and Prof. Allen are currently working to see if using ultrasound waves to modulate brain activity of those who are new to practicing mindfulness helps them achieve the powerful benefits of this practice more quickly. This will lay the groundwork towards developing a hand-held ultrasound brain stimulator, and allowing more people to easily and effectively incorporate mindfulness into their lives. This targeted and focused research will go beyond the apps and other existing technological efforts that aim to facilitate mindfulness today, which often fall short because of their generalized approach.
So far research already shows enticing results: Participants who underwent transcranial focused ultrasound (tFUS), an emerging non-invasive technique to temporarily modulate neural activity, while engaging in meditation reported feeling profound inner peace after just weeks of practice. They said their thoughts flowed more freely, and they felt merged with their surroundings, two long-established characteristics of those who practice long-term mindful meditation.
The researchers say that meditation can improve following the delivery of these low intensity ultrasound waves, which are proven safe, because they help reduce activity in the brain’s default mode network (DMN), a system of brain regions that show less activity when someone is concentrating and focused. In fact, MRI results show that long-term practitioners of mindful meditation have significantly reduced DMN activity. In other words, the ultrasound waves can facilitate and possibly amplify the calming effects of mindful meditation on the brain, creating a cycle where one feels the benefits faster and more significantly, which, in turn leads to more routine practice and more benefits.
Mindfulness tailored to the individual
Our grantees also recognize that embracing a successful routine of mindfulness is not a one -size-fits-all practice. Therefore, their ongoing research also includes a personalized phone app, tailored to each individual to help them overcome their own barriers such as traumatic memories and negative thoughts that might come up with meditation. In addition, the ongoing research includes a wide range of participants, including healthy individuals as well as those suffering from chronic pain, depression and anxiety.
The research could be groundbreaking in that it could eventually lead to a practical solution that will enable more people to incorporate mindfulness into their daily lives. While the research is currently lab-based, relying on a prototype of an ultrasound stimulator, along with regular MRIs, they hope it will lead to an easy-to-use handheld device that can then be used in clinics and wellness retreats later this year, and maybe, someday, by people at home.
Most meaningful life changes require meaningful efforts to get there, and that’s where many people get stuck in our modern, busy world. We believe that technology holds the key to making life-changing practices, including mindful meditation, more accessible and practical, allowing them to truly have deep and long-lasting effects. We are excited to embark on this journey with Dr. Sanguinetti and Prof. Allen and their teams, and we are confident that this partnership will take this technology from the lab out into the world, yielding incredible results for the human experience.
With little exposure to daytime sunlight, and nights brightened by screens and indoor and outdoor lighting, our modern lifestyle has thrown us out of sync with the natural patterns of brightness and darkness that are key to mental and physical wellbeing.
Now, CNS grantees, a neurobiologist, Maria Korman and an occupational therapist Rinatia Maaravi-Hesseg from Ariel University’s occupational therapy department are trying to compensate for indoor lifestyle – induced problems with sleep and psychological wellbeing by using lighting solutions that mimic the natural sunrise.
Can such interventions really make a significant difference? We take you behind the scenes of one project that proves they can.
–
For decades, our modern lifestyles have been keeping us indoors, making us heavily dependent on artificial light. This has thrown our bodies out of sync with the natural cycles of light and darkness that regulate the body’s internal clock, mood, and cognitive function, and are key to basic physiological processes like regulation of body temperature, heart rate, and metabolism. The pandemic, which has led to spending even more time indoors, has only exacerbated this issue, reducing people’s exposure to natural light by 58% during lockdowns. Ultimately, this disconnect with the natural light cycle has resulted in negative psychological and physiological effects.
So when a grant proposal from doctors Maria Korman and Rinatia Maaravi-Hesseg to research how human-centric light technology that mimics sunrise can benefit wellbeing, landed on our doorstep, we knew it was something important that we wanted to fund. The physiological effects of light is an understudied area of science that could have a significant impact on people’s health and mental wellbeing. And there is also a vast commercial potential for such life-changing indoor lighting solutions. In fact, solutions for regulating circadian rhythm in an era of indoor-living and artificial light is a top priority for the wellness tech sector.
“We are always racing against the clock, and feel there is a lack of time, and I believe this is related to the fact that modern society does not rely on natural time cues, especially, changes in light” says Korman, a neurobiologist at Ariel University. “This really hurts our life and our health because under ever-present artificial light we have an illusion of everlasting daytime, which is, of course, devoted to activity. Ultimately, this is reducing our chance to rest and restore. Our goal is to find a smart way out of this race against time using technology to change our light environment. Light is extremely critical to our health, and mental and physical wellbeing.”
Bright nights are not good for us
Differing levels of light have long been a key part of human life. Before the advent of electricity, the timing of the sunrise and sunset determined people’s schedules, including when they slept, worked, socialized and ate. Even when fire, and fuels like gas, emerged to create light at night, these were used in limited quantities due high costs, meaning that nights were still dark, for the most part. Early artificial light sources also had a low blue light component, which is known to promote wakefulness.
“Only in modern times did we become addicted to artificial light,” Korman says, explaining that we constantly desire more and more light. “It’s like sugar, the more you have the more you want.” The omnipresent indoor lighting after sunset, including blue light from LEDs, phone and computer screens, combined with outdoor light from buildings, cars, street lamps and other sources, make nights as bright–or maybe even brighter (think about stadium or stage lighting) –than days.
We essentially have gloomy days with little exposure to sunlight, and overly bright nights. This leads to delayed sleep, lower sleep quality and shortened sleep, and, ultimately, to a multitude of negative health effects, including an increase in rates of depression. These effects are explained by the fact that light-at-night causes the body to produce less melatonin and also directly modulates the activity in brain areas that keep our body clock in sync with the environment.
Naturally Resetting Our Internal Clocks
A possible solution to the negative effects of our indoor lifestyle and resulting misalignment with the natural time, is to expose people to bright artificial light during the morning hours, mimicking the sensation of the natural gradual increase in brightness that starts at sunrise, before your alarm clock rings. Observational studies have found that intense light in the morning is connected to better sleep and lower rates of depression. Korman and Maaravi-Hesseg, a neurobiologist and occupational therapist who also works at Ariel University, will use the grant to expand on previous research, which found that a bedside lamp mimicking the intensity of outdoor light at different times of day, including sunset, darkness, and sunrise, helped people improve their schedules, energy levels and moods.
Indoor light that echoes the course of natural outdoor light throughout the day is part of what Korman calls “the four D’s that lead to improved sleep and wellbeing”: Those include daylight, dim light in the afternoon and evening, a digital diet, or limiting our use of screens at night, and exposure to complete darkness while sleeping.
Korman and Maaravi-Hesseg’s research is especially promising not only because it is rooted in scientific evidence, but also because it is examining solutions that are simple to use. Such unobtrusive interventions like special lamps can easily be used at home and work, in the background; they can be preprogrammed and adjusted to one’s schedules and they don’t require attention. This makes the approach different from existing solutions that require wearing cumbersome blue-light blocking glasses, following the directions of an app or spending large amounts of time sitting under specialized lights.
“We want to improve people’s daily lives without causing inconvenience,” says Maaravi-Hesseg.
Advancing our understanding of how light affects us
Their continuing research will also lead to more scientific understanding of the differences between natural and artificial light, and how light affects health and wellbeing. Studying these relatively neglected aspects of light is important to us at CNS, and for the general advancement of science and technology to help us improve our wellbeing.
Traditionally, most study of light has been related to how it helps us see. But the non-visual aspects of light are clearly critical to human functioning, both psychologically and psychologically. This new research will help clarify our bodies’ relationship with ambient light and develop seamless technological ways to control our light environment in a way that benefits our health and wellbeing. Hopefully, this will light the path out of a lifestyle that so often feels hyperactive, and exhausting; a lifestyle without enough sleep and rest.
Research team Félix Schoeller, PhD, Adam Haar Horowitz and Abhinandan Jain of MIT are using their CNS grant to examine whether the wellbeing benefits of naturally-occurring chills can be reproduced.
Everyone experiences them. Nearly every culture exalts them. The uniquely intense emotional sensation known as chills, frisson, goosebumps, chaire de poule (French), gänsehaut (German), gæsahúð (Icelandic), amagqabi (Xhosa)…it’s seemingly as universal as sneezing or smiling.
Frisson is profoundly tied to meaningful peak emotional experiences—a climactic moment in a movie or a novel, a crescendo in a symphony, a religious experience, an intense interpersonal encounter (including sex). And much research has been conducted on the phenomenon’s psychophysiological benefits—stress reduction, enhanced pleasure and empathy, improved social cognition and even true positive transformative experiences.
But can the benefits of frisson go both ways? What happens if we elicit the physical manifestation of chills, without the psychogenic stimuli that usually causes it? Do we get the same benefits?
In other words, are all goosebumps equal?
Wearable Tech Meets the Chills
To answer this question, CNS grantee Félix Schoeller, PhD, together with Adam Haar Horowitz and Abhinandan Jain of the Fluid Interfaces Group at MIT Media Lab, created wearable technology that replicates, stimulates and enhances psychogenic shivers, AKA chills.
Félix is no stranger to neuroscientific and psychological research, with a large body of original work, collaborations and attributions to his name, notably in the field of interoception – our sense of the internal state of our bodies. With a BFA in filmmaking, and Master’s from the Interdisciplinary School for Advanced Studies in Social Science (EHESS) in Paris, and postdocs at the Centre for Research and Interdisciplinarity in Paris and at the French Institute for Health and Medical Research (INSERM) – Félix was eminently qualified to address the issue.
In this task, he was joined by Adam and Abhi. Adam was a neuroscience researcher at MIT’s McGovern Institute for Brain Research before he became a PhD student and project leader of the Dream Lab, an interdisciplinary research lab focused on dream science that sits under Professor Pattie Maes’ Fluid Interfaces Group at MIT’s Media Lab. Abhi is also a PhD student at the Media Lab studying under Professor Maes. He is trained as an Electronics Engineer and his interests lie in creating technologies for interoceptive interventions.

The team’s hypothesis was simple: they knew that our relationship with our bodies actively informs both our internal emotional life and our perception of the external world. This is known as embodied cognition. Thus, they hypothesized that if organically-occurring psychogenic chills impact cognition, then artificially-generated chills could as well.
The applications – both research and commercial – are intriguing. A device that induces the positive effects of chills could be used to combat anhedonia, the lack of pleasure associated with depression and other mood and affective disorders. It could assist those with impaired empathy or social cognition – autism or alexithymia, for example – in detecting aberrant emotional processing in real time, and even help them respond more appropriately with personalized, sensor-based recommendations of augmented content.
The team’s initial results were very positive. They found that the wearable device did indeed increase reported feelings of empathy and pleasure in subjects. This is highly promising – both for its potential applications to the field of wellbeing, and to scientific inquiry into the underlying mechanisms surrounding chills.
They are now preparing the next round of experiments at Roy Salomon’s Lab of Consciousness and Self at the Gonda Multidisciplinary Brain Centre at Bar-Ilan University. The Salomon lab focuses on the cognitive and neural processes underlying perceptual consciousness and bodily self-consciousness. They use a combination of virtual reality, physiological signals, psychophysics and neuroimaging (EEG, MEG, fMRI) paradigms to study these processes in humans – both in neuro-typical populations and in clinical populations showing deficits in self-representation (e.g. Schizophrenic patients).
Next Research Steps
To further augment the knowledge of frisson, the team extended some prior work Felix had done with network scientist Marc Santolini at CRI Paris to build software to search YouTube for comments on video content mentioning words from the “chills dictionary” – shivers, chills, goosebumps, frisson, etc. From this raw material, they are currently crowdsourcing an effort to create a “chills gold standard” database – asking viewers to record where in each video they experienced chills, the intensity of these chills, and more.

The object of this effort? The team intends to pair their device with this content in an experimental setting. They’re going to create a portable closed-loop system for presenting chills stimuli, combined with psychophysiological sensors and mechanical actuators simulating the sensation of chills – then measuring subject responses in real time.
Why is this relevant? The team believes that artificial frisson sensations could be used to induce emotional processing that will help contextualize the attention paid to interoceptive and exteroceptive sensations. For example, in children with autism, artificial sensations that did or did not produce psychogenic shivers could be used to assess interoceptive sensitivity. Similarly, individuals with alexithymia could be more effectively assessed – quantifying the extent to which they recognize chills-inducing and non-chills-inducing content, and their differential event-related responses.

The Bottom Line
In answer to our question: it is entirely possible that a goosebump is a goosebump is a goosebump.
In other words, the psychophysiological benefits of psychogenic frisson appear to be similar to those from artificially-induced chills. The pleasure and wellbeing naturally derived from peak emotional experiences may be duplicatable. Moreover, the ability to discern whether an experience is or is not emotionally meaningful may be quantifiable.
At the very least, the team expects their device and research to offer a deeper understanding of the role that bodily sensations play in brain function. Yet ultimately, this enquiry could serve as a game-changing basis for commercial and clinical tools that effectively interface with the body to improve health and wellbeing.
At CNS, we are committed to accelerating profound discoveries and cutting-edge technologies to drive impact across broad areas of mental wellbeing. Félix, Adam and Abhi’s project is a perfect example of the great things that can happen when cutting edge technology and academic research join to find viable, effective solutions. We are thrilled to be supporting this team and look forward to sharing the results of their project!
